Why in news?
- Some critical weaknesses in the country’s health system can come in the way of a credible strategy to combat COVID-19
- Much concern about the novel coronavirus in India is understandably about the number of cases and related deaths.
Details
- It is important to remember that the vast majority (80%) of COVID-19 cases will be mild.
- The estimated mortality rate varies considerably between 3% to 0.25% of cases, and is much higher among the elderly.
- Notably, wealthier countries with stronger and better financed health systems such as Italy and China have struggled with containing COVID-19.
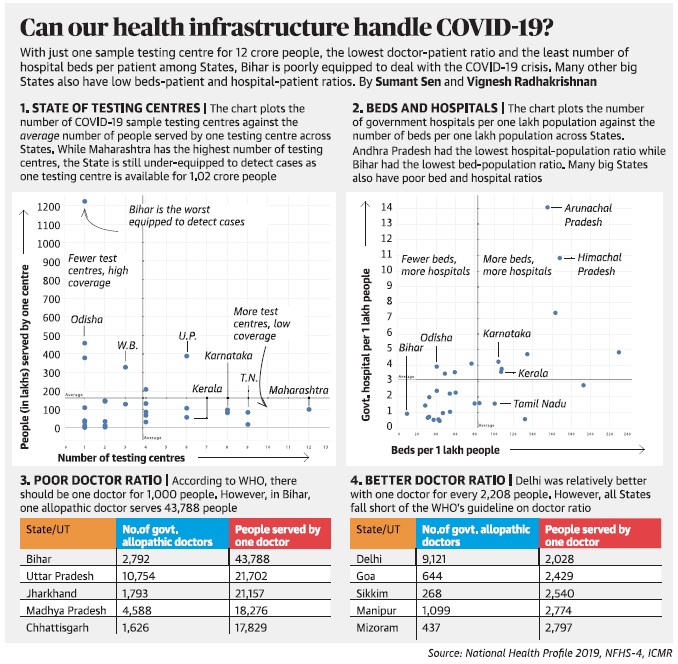
- As such, it is prudent to understand how well India’s health system can respond to COVID-19, especially since it is unclear how long this disease will persist. We believe that there are some critical weaknesses in India’s health system that can prevent a credible response to COVID-19.
Ramping up hospital capacity
- Addressing the scarcity of hospital and intensive care unit (ICU) beds in India is critical for providing clinical support to severe COVID-19 cases.
- Without flattening India’s COVID-19 epidemic curve, our current hospital capacity is so low that it will be quickly overwhelmed if infections surge.
- It is critically important that India puts in place a strategy to ramp up hospital and ICU capacity, as well as provision for essential equipment such as ventilators and personal protective equipment for health workers. In both China and Italy, hospitals were rapidly constructed to accommodate infected patients.
- Tapping the resources in the private sector is particularly important. India’s health system is highly privatised and most of the country’s health-care capacity in terms of human resources, hospital beds, laboratories, and diagnostic centres is in the private sector.
- Recognising this, several State governments have initiated action, such as enlisting private laboratories for testing and using the private hospital bed capacity to treat positive patients.
- More of this is needed, as well as, engaging private hospitals in planning and coordinating the COVID-19 response.
Health workers are crucial
- Health-care workers are a critical resource for the COVID-19 response. They go into communities to carry out preventive care, trace potentially exposed people, and treat the infected.
- Primary-care providers, whether they are formally trained (e.g. medical officers, nurses, auxiliary nurse and midwives, pharmacists), or lay workers (accredited social health activists) or informal workers (rural (not registered) medical practitioners, or RMPs, drug shops) will likely be the first contact health workers for COVID-19 patients.
- Health workers also take on a disproportionate share of infections. Health worker safety is particularly important for India because it already faces a shortage of doctors and nurses.
Conclusion
- India like other countries faces important health system challenges in mounting a credible response to COVID-19. Many of these issues are not new.
- Addressing these health system issues will require much effort, financing, and, in some cases, not even entirely possible to remedy in the near future.
- How India deals with these health system issues in the days to come will make all the difference.